Vitamax Healthcare Private Limited
Vitamax Healthcare Private Limited is a Private incorporated on 18 July 2008. It is classified as Non-govt company and is registered at Registrar of Companies, Gwalior

Products
AMIKACIN SULPHATE INJECTION
Amikacin is a man-made aminoglycoside antibiotic. It is similar to tobramycin and gentamicin. Amikacin binds to components of bacteria that produce important bacterial proteins, blocking protein synthesis which eventually leads to stopping further bacterial growth. Amikacin is used to treat infections caused by bacteria that are resistant to gentamicin and tobramycin. Amikacin treats infections caused by gram-negative bacteria such as Pseudomonas species, Escherichia coli, Providencia species, Indole-positive and indole-negative Proteus species, Klebsiella-Enterobacter-Serratia species, and Acinetobacter. Amikacin is also used in certain staphylococcal infections as well.
ARTEMETHER INJECTION
Artemether 80 mg injection Augmentin is and what it General information Group: antimalarial agent Oily solution for injection 80 mg in 1-ml ampoule Artemether is a lipid-soluble methyl ether of dihydroartemisinin which has very rapid schizontocidal activity against blood forms of P. falciparum and P. vivax. After intramuscular administration, peak plasma concentrations are attained within about 6 hours. Artemether has been reported to clear fever in severe falciparum malaria within 30-84 hours. Clinical information Uses Treatment of slide-confirmed severe falciparum malaria in areas where there is evidence that quinine is ineffective. Radical cure should then be effected with a full dose of an effective oral antimalarial such as mefloquine. Dosage and administration Adults and children over 6 months: 3.2 mg/kg as a loading dose by intramuscular injection, followed by 1.6 mg/kg daily until the patient is able to tolerate oral medication or for a maximum of 7 days. Precautions Artemether should be used for the treatment of severe falciparum malaria only where there is evidence that the antimalarial efficacy of quinine is declining. For children, since the injected volumes will be small, it is advisable to use a 1-ml syringe to ensure that the correct dose is given. Use in pregnancy Little experience has been gained with the use of this drug in pregnancy but it should not be withheld if it is considered life-saving to the mother. Adverse effects Neurotoxicity has been observed in animal studies but not in humans. Cardiotoxicity has been observed following administration of high doses of artemether. Storage The oily preparation should be stored in tightly closed containers, protected from light. This information is a summary only. It does not contain all information about this medicine. If you would like more information about the medicine you are taking, check with your doctor or other health care provider. No rights can be derived from the information provided in this medical.
BETAMETHASONE INJECTION
Betamethasone Injection belongs to a group of medicines called steroids. Their full name is corticosteroids.
These corticosteroids occur naturally in the body and help to maintain health and well being. Boosting your body with extra corticosteroids (such as Betamethasone Injection) is an effective way to treat various illnesses involving inflammation in the body. Betamethasone Injection reduces this inflammation, which could otherwise go on making your condition worse. You must use this medicine regularly to get maximum benefit from it.
Many different conditions can be improved by the use of corticosteroids, as they reduce inflammation (redness, tenderness, heat and swelling) in the body.
Betamethasone Injection is used:
- to treat asthma
- to treat severe allergic reactions including reactions to drugs
- to treat local inflammation e.g. of joints, tendons or the eye
- as replacement for the body’s naturally occurring corticosteroid hormones when these are reduced or absent
- to treat severe shock, (collapse) due to surgery, injury or overwhelming infection.
Corticosteroids are also used to help prevent organ transplant rejection following organ transplant surgery.

CYANOCOBALAMIN INJECTION
Indications for Cyanocobalamin injection:
Vit. B12 deficiencies due to malabsorption. Pernicious anemia. Vit. B12 absorption test (Schilling test).
Give by IM or deep SC inj. Pernicious anemia: 100mcg daily for 6–7 days; then 100mcg every other day for 7 doses; then every 3–4 days for 2–3 weeks; then 100mcg monthly for life. Deficiencies due to malabsorption: if severe, may need to treat like pernicious anemia; use oral preparations for chronic treatment. Schilling test: 1000mcg.
Contraindications:
Sensitivity to cobalt.
Warnings/Precautions:
Hereditary optic nerve atrophy (Leber’s disease). Severe megaloblastic anemia (intense treatment may lead to hypokalemia and death). Monitor potassium for first 48 hours; replace if needed. Obtain hematocrit, reticulocyte count, Vit. B12, folate, and iron levels before and during treatment. Reevaluate periodically. Premature infants. Renal impairment (possible aluminum toxicity). Folic acid use may mask B12 deficiency. Pregnancy (Cat. C).
Interactions:
Antibiotics, methotrexate, pyrimethamine interfere with Vit. B12 diagnostic tests. Colchicine, para-aminosalicylic acid, heavy alcohol intake for >2 weeks may produce malabsorption of Vit. B12.
Adverse Reactions:
Pulmonary edema, CHF, vascular thrombosis, polycythemia vera, transient diarrhea, itching, transitory exanthema; anaphylactic shock (may be fatal; do test dose if hypersensitivity suspected).
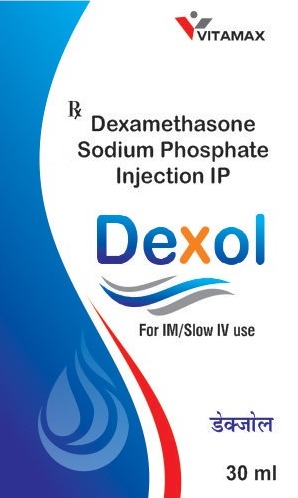
DEXAMETASONE SODIUM PHOSPHATE INJECTION
Dexamethasone is used to treat many inflammatory and autoimmune conditions, such as rheumatoid arthritis and bronchospasm. Idiopathic thrombocytopenic purpura, a decrease in numbers of platelets due to an immune problem, responds to 40 mg daily for four days; it may be administered in 14-day cycles. It is unclear whether dexamethasone in this condition is significantly better than other glucocorticoids.
It is also given in small amounts before and/or after some forms of dental surgery, such as the extraction of the wisdom teeth, an operation which often leaves the patient with puffy, swollen cheeks.]
Dexamethasone is commonly given as a treatment for croup in children, as a single dose can reduce the swelling of the airway to improve breathing and reduce discomfort.
It is injected into the heel when treating plantar fasciitis, sometimes in conjunction with triamcinolone acetonide.
It is useful to counteract allergic anaphylactic shock, if given in high doses.]
Dexamethasone intravitreal steroid implants have been approved by the FDA to treat ocular conditions such as diabetic macular edema, central retinal vein occlusion, and uveitis.
Dexamethasone has also been used with antibiotics to treat acute endophthalmitis.
Dexamethasone is used in transvenous screw-in cardiac pacing leads to minimize the inflammatory response of the myocardium. The steroid is released into the myocardium as soon as the screw is extended and can play a significant role in minimizing the acute pacing threshold due to the reduction of inflammatory response. The typical quantity present in a lead tip is less than 1.0 mg.]
Dexamethasone may be administered before antibiotics in cases of bacterial meningitis. It acts to reduce the inflammatory response of the body to the bacteria killed by the antibiotics (bacterial death releases proinflammatory mediators that can cause a response which is harmful), thus reducing hearing loss and neurological damage.
DICLOFENAC SODIUM INJECTION
Therapeutic action
Non-steroidal anti-inflammatory drug (NSAID), analgesic for deep IM injection or IV infusion
Indications
Moderate pain due to inflammation (acute sciatic neuralgia, renal colic, postoperative pain, etc.)
Dosage
– Adult : 75 mg by deep IM injection, to be repeated after 6 hours if necessary
– For postoperative pain, may be administered by infusion: 75 mg over 30 to 120 minutes, to be repeated after 4 to 6 hours if necessary.
– Do not exceed 150 mg in 24 hours.
Duration
– Maximum 2 days; change to oral treatment with an analgesic, e.g. ibuprofen or paracetamol, as soon as possible.
Contra-indications, adverse effects, precautions
– Do not administer to patients with allergy to NSAID (aspirin, ibuprofen, etc.), peptic ulcer, coagulation defects, haemorrhage, surgery with risk of major blood loss, severe renal, hepatic or cardiac impairment, severe malnutrition, uncorrected dehydration or hypovolaemia, asthma, severe infection.
– May cause: local reactions at the injection site, renal impairment, gastrointestinal disturbances, allergic reactions (skin rash, bronchospasm).
– Administer with caution and carefully monitor use in older patients or patients with cardiovascular disorders (hypertension, diabetes, etc.).
– Do not combine with other NSAID (aspirin, ibuprofen, etc.), diuretics, anticoagulants.
– Pregnancy: CONTRA-INDICATED
– Breast-feeding: CONTRA-INDICATED
Remarks
– For infusion, use a solution of 5% glucose or 0.9% sodium chloride and add 0.5 ml of 8.4% sodium bicarbonate per 500 ml.
– Diclofenac is not included in the WHO list of essential medicines.
– Storage: below 25 °C
GENTAMICIN SULPHATE INJECTION
Gentamicin is normally given by the intramuscular route, but can be given intravenously when intramuscular administration is not feasible, e.g. in shocked or severely burned patients. When given intravenously, the prescribed dose should be administered slowly over no less than 3 minutes directly into a vein or into the rubber tubing of a giving set. Rapid, direct intravenous administration may give rise, initially, to potentially neurotoxic concentrations and it is essential that the prescribed dose is administered over the recommended period of time. Alternatively the prescribed dose should be dissolved in up to 100 ml of normal saline or 5% glucose in water, but not solutions containing bicarbonate (see Incompatibilities P6B, 7h), and the solution infused over no longer than 20 minutes.
The same dosage schedule is recommended for intramuscular and intravenous dosing. Dosage is related to the severity of infection, the age of the patient and the patient’s renal function.
The daily dose recommended in children, adolescents and adults with normal renal function, is 3-6 mg/kg body weight per day as 1 (preferred) up to 2 single doses.
The daily dose in infants after the first month of life is 4.5-7.5 mg/kg body weight per day as 1 (preferred) up to 2 single doses.
The daily dose in newborns is 4-7 mg/kg body weight per day. Due to the longer half-life, newborns are given the required daily dose in 1 single dose.
In impaired renal function, the recommended daily dose has to be decreased and adjusted to the renal function

QUININE HYDROCHLORIDE INJECTION
Therapeutic action – Antimalarial
Indications
– Alternative to injectable artesunate, when it is not available, in the treatment of severe malaria
Forms and strengths, route of administration
– 600 mg of quinine dihydrochloride in 2 ml ampoule (300 mg/ml), to be diluted in 5% glucose, for slow infusion. NEVER ADMINISTER BY IV INJECTION.
Dosage
The dosage is expressed in terms of salt:
– Child and adult:
• loading dose: 20 mg/kg administered over 4 hours, then keep the vein open with an infusion of 5% glucose over 4 hours
• maintenance dose: 8 hours after the start of the loading dose, 10 mg/kg every 8 hours (alternate quinine over 4 hours and 5% glucose over 4 hours)
For adults, administer each dose of quinine in 250 ml. For children under 20 kg, administer each dose of quinine in a volume of 10 ml/kg.
Do not administer a loading dose to patients who have received oral quinine or mefloquine within the previous 24 hours: start with maintenance dose.
Duration– Treat parenterally for at least 24 hours, then, if the patient can tolerate the oral route, change to a complete 3-day course of an artemisinin-based combination (or if not available oral quinine to complete 7 days of quinine treatment). If not, continue parenteral treatment until the patient can change to oral route (without exceeding 7 days of parenteral treatment).
Contra-indications, adverse effects, precautions
– May cause: hypoglycaemia; auditory and visual disturbances, cardiac disorders (especially in the event of overdose), hypersensitivity reactions, cardiac depression if injected undiluted by IV route.
– In patients with acute renal failure, reduce the dose by one-third if the parenteral treatment lasts more than 48 hours.
– Monitor blood glucose (reagent strip test).
– Do not administer simultaneously with mefloquine (risk of seizures, cardiac toxicity). Administer mefloquine 12 hours after the last dose of quinine.
– Pregnancy: no contra-indication. The risk of quinine-related hypoglycaemia is very high in pregnant women.
– Breast-feeding: no contra-indication
Remarks
– 10 mg quinine dihydrochloride = 8 mg quinine base.
– Administration by IM deep injection (into the anterior thigh only) is possible when infusion cannot be performed (e.g. before transferring a patient). However this may cause numerous complications. Doses are the same as for the IV route. Quinine should be diluted (1/2 or 1/5). For the loading dose, administer half the dose into each thigh.
– Storage: below 25 °C –
